Radical Vaccine Strategy Could Help Quash Parasite Afflicting Millions
Using viruses that infect bacteria to detect proteins sprouted by a notorious parasite, scientists have honed in on possible vaccine targets for schistosomiasis, a neglected tropical disease that currently affects an estimated 600 million people worldwide, causing 280,000 deaths per year.
The Brazil-based team harnessed a method called phage display, which was first described in the 1980s, to probe Schistosoma parasites that cause the disease, faster and more comprehensively than previous, sluggish research efforts could muster.
“You often hear the argument that a schistosomiasis vaccine isn’t feasible,” says Sergio Verjovski-Almeida, a molecular biologist at the Butantan Institute in São Paulo, Brazil, and senior author of the study.
But every pathogen has tell-tale markings that a person’s immune system can learn to recognize, if primed with a vaccine. The trick is finding which protein to target, to ignite a strong immune response.
Screening disease-causing pathogens for potential vaccine targets is a costly and time-consuming exercise that usually only reveals a small fraction of a pathogen’s distinctive proteins, expressed on its outer surface.
There’s also little financial incentive for pharmaceutical companies to invest in vaccine development for tropical diseases affecting the world’s poorest people if they can’t recoup their costs – hence why these diseases have been neglected for so long.
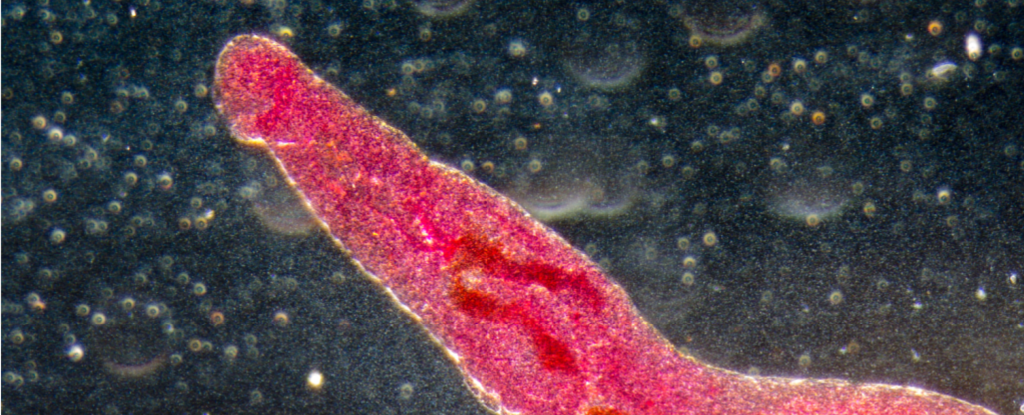
Schistosomiasis, also known as snail fever or water belly, is caused by parasitic worms that infect snails as well as humans. It spreads in areas with poor hygiene and sanitation where water has been contaminated with the worm’s eggs, which hatch to form larvae that penetrate people’s skin.

Once in a person’s bloodstream, the larvae transform into adult worms that lodge in the veins of the intestines, causing disease two to six weeks after the initial infection.
To expose the beastly parasites, the Brazilian team turned to phage display, a technique that has come to the fore in recent years, used to profile pathogens causing Chagas disease, Leptospirosis and even COVID-19.
“Phage display had never been deployed for this purpose in research on parasitic diseases, which normally involves preselection of a few targets for testing of candidate vaccines,” explains Butantan Institute molecular biologist Murilo Sena Amaral.
The method involves using bacteriophages to study protein-protein interactions. In this case, the researchers assembled an army of bacteriophages engineered to carry snippets of DNA encoding all 11,641 known proteins of Schistosoma mansoni worms from every stage of their life cycle.
The bacteriophages displaying these Schistosoma proteins were then incubated with blood plasma samples from 10 rhesus macaques infected with S. mansoni, one of several Schistosoma worm species that cause different forms of the disease.
If a bacteriophage met its match in antibodies produced by the rhesus monkeys in response to their infection, those phages could be separated out and analyzed.
In total, the researchers detected 99.6 percent of the 119,747 DNA sequences encoding Schistosoma proteins in the monkey’s plasma – and found some were particularly abundant, suggesting they are key proteins driving the immune response to Schistosoma infections.
“Our discoveries have revealed a great deal of the immune response and opened up promising prospects for the development of an effective vaccine,” Verjovski-Almeida says.
For instance, the researchers found that extracellular parasite proteins were more prominent in the early stages of infection, whereas intracellular proteins became more pronounced later on.
Bear in mind, however, that this protein identification is just the first milestone in a long process to develop a working vaccine. The proteins of interest, or strips of their genetic codes, need to be packaged up with an adjuvant, an ingredient used to boost immune responses to vaccines, and tested to see if it works in formulation.
A pilot vaccination assay in mice testing a selection of the most promising protein candidates, pooled together but not packaged like a typical vaccine, did succeed in reducing the number of worms the immunized animals carried.
So the early results are encouraging, but the track record of schistosomiasis vaccines tells of the stark reality of vaccine development.
To date, most protein-based vaccines for schistosomiasis have failed in clinical trials to elicit a strong immune response or protect against the disease.
Only one vaccine candidate has reached the final phase of clinical trial testing, where data showed it was safe but not effective. Hopes are pinned on another vaccine not far behind in phase II testing, although it could face the same fate.
The good thing is, after this study, researchers have lots more candidates to explore if one fails.
The study has been published in npj Vaccines.
Source : 1