Considering the crucial role that the information generated from clinical trials play in the approval of new drugs, biological, and medical devices, it is only logical that the data garnered from them is accurate, reliable, reproducible, and traceable as well as in a format that is suitable across various platforms and regulatory systems. The increase in the globalization of clinical trials and the conduct of multi-centre trials in different regions of the world with varying data capture formats and regulatory requirements, makes it necessary to develop systems that allow for data sharing, integration, comparison, and analysis in a standard format using terminologies that are understandable across the globe. Furthermore, the increasing use of real-world evidence (RWE) to support regulatory decision-making also requires that diverse data from various sources such as electronic health records (EHRs), imaging studies, wearable sensors, insurance claims, etc. be standardized to a consistent format.
Clinical data standardization forms an important component of clinical studies and helps increase the usefulness, applicability, and allows for sharing and dissemination of information obtained from them. According to the United States Food and Drug Administration (FDA) data standards provide a consistent meaning to data shared among different information systems, programs, and agencies throughout the product’s lifecycle. These include representation, format, definition, structuring, tagging, transmission, manipulation, use, and management of data. To facilitate the exchange of information across different regulatory platforms, the FDA has worked with the Clinical Data Interchange Standards Consortium (CDISC) to receive, process, review, and archive submissions more effectively and CDISC standards are required for regulatory submissions to the FDA. Thus, clinical data standardization allows for interoperability, data consistency, easier comparisons and analysis, and better patient care based on sound decision-making.
The FDA guidance document entitled “Providing Regulatory Submissions in Electronic Format-Standardized Study Data” released in June 2021 describes technical requirements for submission of standardized data in electronic format for investigational new drug applications (IND), new drug applications (NDA), abbreviated new drug applications (ANDA), and biologics license application (BLA).
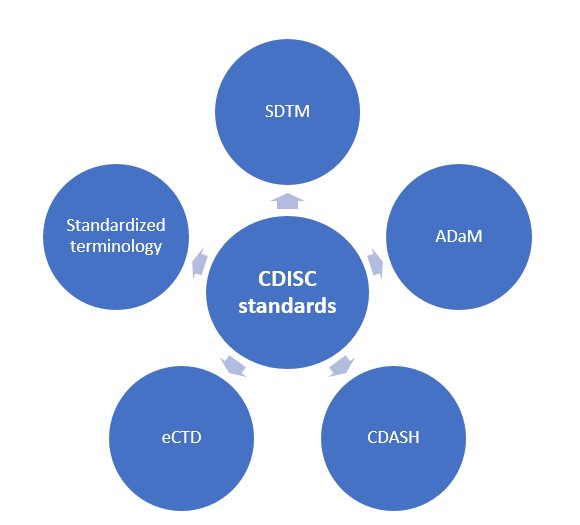
The FDA uses the following CDISC and other systems for data submission, organization, and analysis across various steps of the clinical trial process form data collection to submission as shown below:
Study Data Tabulation Model (SDTM):
This is a set of standards for organizing and formatting data to streamline processes in collection, management, analysis, and reporting. SDTM organizes raw data from clinical trials into various domains such as demographics, adverse events, interventions, concomitant medications, medical history, physical examinations, vitals, laboratory tests, trial designs, etc. and ensures consistency in data formatting that can be uniformly reviewed and is mandatory for regulatory submissions to the FDA. It supports regulatory review and approval processes and provides data for meta-analysis and other research purposes.
Analysis Data Model (ADaM):
This provides a standard data structure intended to support analysis and involves extraction, transformation, and derivations and works together with SDTM to support data submissions to allow data to be imported from SDTM data sets to an analysis ready ADaM format. It helps to link any data derived with the original values entered in SDTM datasets and thus ensures traceability of the data. Furthermore, by providing structured data sets and variable naming conventions, ADaM provides reproducibility and consistency in the data as well.
Clinical Data Acquisition Standards Harmonization (CDASH):
These are standardized data collection guidelines for clinical research and are a part of CDISC SDTM. The aim of CDASH is to develop content standards for a basic set of global case report form (CRF) fields and create data collection tools that are clear, understandable, and precise. CDASH is particularly important in multi-centre trials as they allow uniformity in data collection thereby facilitating analysis and an improvement in data collection efficiency.
Electronic Common Technical Document (eCTD):
The eCTD is a standard format for submitting applications, amendments, supplements, and reports to the FDA’s Centre for Drug Evaluation and Research (CDER) and CBER. It contains non clinical, clinical, and chemistry, manufacturing, and controls, and administrative information for the drug substance and drug product in a standardized format that helps in streamlining the submission process and helps in the review and approval process for various phases of clinical trials. Making this process electronic rather than paper-based has the potential to improve accessibility and traceability and saves on physical storage requirements. Any amendments and updates to the information can be subsequently traced with ease and cross-referencing between different sections is easy using the electronic submission process.
Standardized terminology:
To maintain consistency and uniformity in medical terminology which can be complex and variable, the FDA encourages the use of standardized coding and vocabulary systems in data standardization. This helps the FDA analyze information with ease and hasten the review process. The FDA supports the use of Medical Dictionary for Regulatory Activities (MedRA) for coding of adverse events, CDISC terminologies for data standardization in the submission process, the NATIONAL Drug File (NDF) for information related to drug and formulations, and the WHODrug which is a global medical dictionary.
Thus, combining all the above elements will help in data standardization that is required for regulatory submissions to the FDA. Embracing data standards using these criteria will help ease the regulatory burden and be beneficial to both sponsor/investigators and regulatory agencies.
Read More:
Future Trends in Clinical Data Management
References
- Data Standards and Terminology Standards for Information Submitted to CDRH | FDA
- Global Regulatory Requirements | CDISC
- Clinical Data Acquisition Standards Harmonization importance and benefits in clinical data management – PMC (nih.gov)
- Electronic Common Technical Document (eCTD) | FDA
- eSubmission: Projects (europa.eu)
- WHODrug: A Global, Validated and Updated Dictionary for Medicinal Information – PMC (nih.gov)