This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
AI supports doctors' hard decisions on cardiac arrest
When patients receive care after cardiac arrest, doctors can now—by entering patient data in a web-based app—find out how thousands of similar patients have fared. Researchers at the University of Gothenburg have developed three such systems of decision support for cardiac arrest that may, in the future, make a major difference to doctors' work.
One of these decision support tools (SCARS-1), now published, is downloadable free of charge from the Gothenburg Cardiac Arrest Machine Learning Studies website. However, results from the algorithm must be interpreted by people with the right skills. AI-based decision support is expanding strongly in many areas of health care, and extensive discussions are underway on how care services and patients alike can benefit most from it.
The app accesses data from the Swedish Cardiopulmonary Resuscitation Register on tens of thousands of patient cases. The University of Gothenburg researchers have used an advanced form of machine learning to teach clinical prediction models to recognize various factors that have affected previous outcomes. The algorithms take into account numerous factors that relate, for example, to the cardiac arrest, treatment provided, previous ill-health, medication and socioeconomic status.
New evidence-based methods
It will be a few years before official recommendations for cardiac arrest are likely to include AI-based decision support, but doctors are free to use these prediction models and other new, evidence-based methods. The research group working on decision support for cardiac arrest is headed by Araz Rawshani, a researcher at the University's Sahlgrenska Academy and resident physician in cardiology at Sahlgrenska University Hospital.
"Both I and several of my colleagues who treat emergency patients with cardiac arrest have already started using the prediction models as part of our process for deciding on the level of care. The answer from these tools often means we get confirmation of views we've already arrived at. Still, it helps us not to subject patients to painful treatment that is very unlikely to be of benefit to the patient, while saving care resources," Rawshani says.
Highly accurate
To date, the research group has published two decision support tools. One clinical prediction model, known as SCARS-1, is presented in eBioMedicine. This model indicates whether a new patient case resembles other previous cases, where patients had survived or died 30 days after their cardiac arrest.
The model's accuracy is unusually high. Based on the ten most significant factors alone, the model has a sensitivity of 95% and a specificity of 89%. The "AUC-ROC value" (ROC being the receiver operating characteristic curve for the model and AUC the area under the ROC curve) for this model is 0.97. The highest possible AUC-ROC value is 1.0 and the threshold for a clinically relevant model is 0.7.
One piece of the puzzle
This decision support was developed by Fredrik Hessulf, a doctoral student at Sahlgrenska Academy, University of Gothenburg, and anesthesiologist at Sahlgrenska University Hospital/Mölndal.
"This decision support is one of several pieces in a big puzzle: the doctor's overall assessment of a patient. We have many different factors to consider in deciding whether to go ahead with cardiopulmonary resuscitation. It's a highly demanding treatment that we should give only to patients who will benefit from it and be able, after their hospital stay, to lead a life of value to themselves," Hessulf says.
This form of support is based on 393 factors affecting patients' chances of surviving their cardiac arrest for 30 days after the event. The model's high accuracy may be explained by the huge number of patient cases (roughly 55,000) on which the algorithm is based and the fact that ten of the nearly 400 factors have been found to impact heavily on survival. By far the most important factor was whether the heart regained a viable cardiac rhythm again after the patient's admission to the emergency department.
Risk of new cardiac arrest
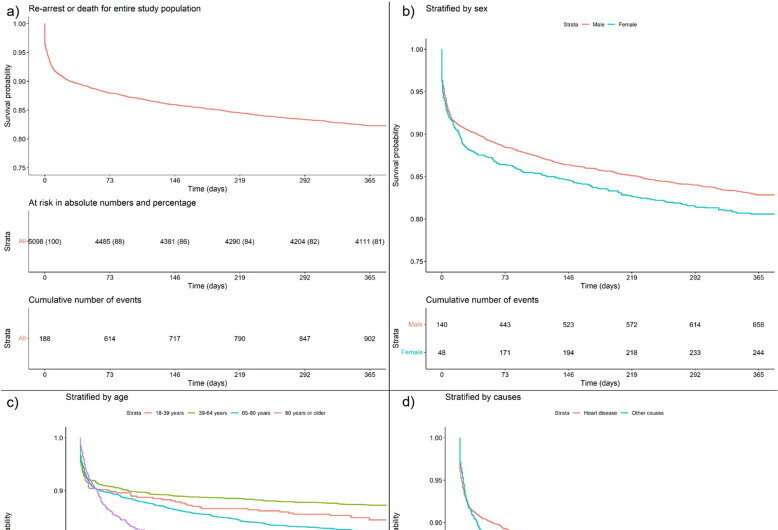
The second decision support tool published has been presented in the journal Resuscitation. This tool is based on data from patients who survived their out-of-hospital cardiac arrest until they were discharged from hospital. The predictive models are based on 886 factors in 5,098 patient cases from the Swedish Cardiopulmonary Resuscitation Register. This tool is partly aimed at helping doctors identify which patients are at risk of another cardiac arrest or death within a year of discharge from hospital following their cardiac arrest. It also aims to highlight which factors are important for long-term survival after cardiac arrest—an aspect of the subject area that has not been well studied.
"The accuracy of this tool is reasonably good. It can predict with about 70% reliability whether the patient will die, or will have had another cardiac arrest, within a year. Like Fredrik's tool, this one has the advantage that just a few factors can predict outcome almost as well as the model with several hundred variables," says Gustaf Hellsén, the research doctor who developed this decision support tool.
"We hope to succeed in developing this prediction model, so as to enhance its precision. Today, it can already serve as support for doctors in identifying factors with an important bearing on survival among cardiac arrest patients who are to be discharged from hospital."
Three decision support tools for different aspects of cardiac arrest
Currently, the SCARS-1 tool (developed by Fredrik Hessulf, addressing survival and neurological function 30 days after cardiac arrest) is available to use as an online app. SCARS-2 (developed by Gustaf Hellsén and designed to support decisions on the risk of new cardiac arrest after discharge) will be launched shortly. During 2023, publication of SCARS-3 (for in-hospital cardiac arrest) is also planned.
Doctors and other health professionals can read more about these decision support tools and download the applications at http://gocares.se.
More information: Fredrik Hessulf et al, Predicting survival and neurological outcome in out-of-hospital cardiac arrest using machine learning: the SCARS model, eBioMedicine (2023). DOI: 10.1016/j.ebiom.2023.104464
Gustaf Hellsén et al, Predicting recurrent cardiac arrest in individuals surviving Out-of-Hospital cardiac arrest, Resuscitation (2022). DOI: 10.1016/j.resuscitation.2022.109678



















