Early data shows Russia's Sputnik V COVID-19 vaccine produces immune response
A trial of Russia’s Sputnik V coronavirus vaccine has shown the jab produces an immune response, although the study was too small to produce conclusive findings, particularly on safety.
Preliminary results published in The Lancet are from a non-randomised phase 1/2 trial of 76 people aged 18-60, which found an antibody response within 21 days and no serious adverse events after 42 days. The vaccine also produced a T-cell response within 28 days, a secondary outcome.
And although there were no serious adverse events detected in the two formulations, the small sample size means that it’s impossible to draw conclusions about its safety until data from a larger trial are available.
The World Health Organization has placed the vaccine in third place on its list of 34 coronavirus vaccines in clinical trials, and the vaccine's name refers to the Soviet-era space programme that won the 'space race' by placing the first satellite into orbit.
But there are concerns that Russia has rushed development of the vaccine to claim a political victory in the race to get a vaccine approved.
Leading respiratory doctor Professor Alexander Chuchalin has quit the country's ethics council in protest following approval by Russian regulators, which have green-lighted a phase 3 trial that is expected to include 40,000 volunteers from different age and risk groups.
The two-part vaccine includes two adenovirus vectors – recombinant human adenovirus type 26 (rAd26-S) and recombinant human adenovirus type 5 (rAd5-S) – which have been modified to express the SARS-CoV-2 spike protein.
The adenoviruses are also weakened so that they cannot replicate in human cells and cannot cause disease – adenovirus usually causes the common cold.
Dr Denis Logunov, of the Gamelaya National Research Centre for Epidemiology and Microbiology in Russia, said the vaccine used two different virus vectors to prevent the body producing an immune response and blocking the second booster jab.
He said: “Booster vaccinations that use the same adenovirus vector might not produce an effective response, because the immune system may recognise and attack the vector.
“This would block the vaccine from entering people’s cells and teaching the body to recognise and attack SARS-CoV-2. For our vaccine, we use two different adenovirus vectors in a bid to avoid the immune system becoming immune to the vector.”
The freeze-dried vaccine was trialled in a branch of the Burdenko Hospital, an agency of Russia’s defence ministry, in civilian patients who self-isolated as soon as they were registered and remained in hospital for 28 days after the first vaccination.
In the phase 1 part of the trial, participants received one component of the two-part vaccine. In the phase 2 trial, which began no earlier than five days after the phase 1 trial began, participants received the full two-part vaccine.
The most common adverse events were pain at injection site (44/76 participants – 58%), hyperthermia (high temperature – 38/76 – 50%), headache (32/76 – 42%), asthenia (weakness or lack of energy – 21/76 – 28%), and muscle and joint pain (18/76 – 24%).
Most adverse events were mild, and no serious adverse events were detected within 42 days of vaccination. The authors note that these adverse effects are characteristic of those seen with other vaccines, particularly those based on recombinant viral vectors.
All participants in the phase 2 trials (40 participants) produced antibodies against the SARS-CoV-2 spike protein.
Authors said the antibody responses produced by the vaccine appeared to be stronger in those taking the vaccine than in patients recovering from the disease.
Professor Alexander Gintsburg, N F Gamaleya National Research Centre for Epidemiology and Microbiology, Russia, said: “Unprecedented measures have been taken to develop a COVID-19 vaccine in Russia.
Preclinical and clinical studies have made it possible to provisionally approve the vaccine under the current Russian coronavirus regulations.
“This provisional licensure requires a large-scale study, allows vaccination in a consented general population in the context of a phase 3 trial, allows the vaccine to be brought into use in a population under strict pharmacovigilance, and to provide vaccination of risk groups.”
Lead author Dr Naor Bar-Zeev, International Vaccine Access Center, Johns Hopkins Bloomberg School of Public Health, US who was not involved in the study, said: “Similar to these studies before it, Logunov and colleagues’ studies are encouraging but small.
“The immunogenicity bodes well, although nothing can be inferred on immunogenicity in older age groups, and clinical efficacy for any COVID-19 vaccine has not yet been shown.
“Showing safety will be crucial with COVID-19 vaccines, not only for vaccine acceptance but also for trust in vaccination broadly.
“Since vaccines are given to healthy people and, during the COVID-19 pandemic, potentially to everyone after approval following phase 3 trials, safety is paramount.”
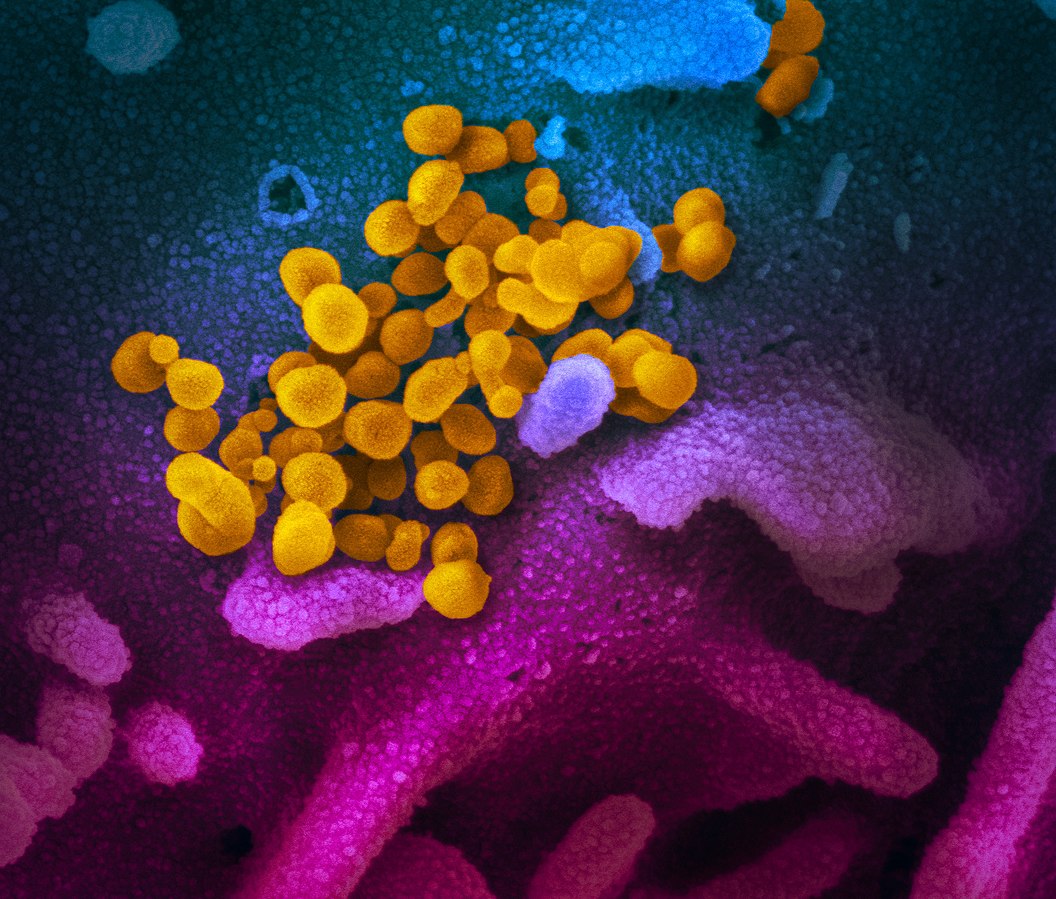
Feature image courtesy of Rocky Mountain Laboratories/NIH













