Historical events such as the sulfanilamide elixir tragedy that resulted in the mass poisoning and the deaths of hundreds of patients in the 1930s and the thalidomide scandal which caused birth defects and mortality of babies prompted the United States Congress to enact legislation pertaining to the regulation of drugs, medical devices, biologicals, and food articles that involved an extensive safety evaluation of products prior to marketing authorization. The Federal Food, Drug, and Cosmetic Act of 1938 was enacted with the primary purpose of consumer protection in mind and to ensure the safety and well-being of all people consuming or utilizing the products mentioned in the Act. Several years later, the United States remains as having the strictest regulations and laws relating to clinical research in human subjects, and rightly so as patient health, well-being, and integrity are of paramount importance in all aspects of Good Clinical Practice (GCP) guidelines.
Title 21 is a part of the Code of Federal Regulations (21 USC §§ 301-302) that governs food and drugs within the U.S. for the Food and Drug Administration (FDA), Drug Enforcement Administration (DEA), and the Office of National Drug Control Policy (ONDCP) and is divided into three chapters of which Chapter 1 is related the FDA. The FDA is the federal agency that is responsible for the regulation of drugs and medical devices allowing investigational drugs to enter interstate commerce and finally approving their market availability as well as post-marketing surveillance. The FDA oversees and ensures compliance with the FD&C Act and enforces other laws of the Public Health Service (PHS) Act as well.
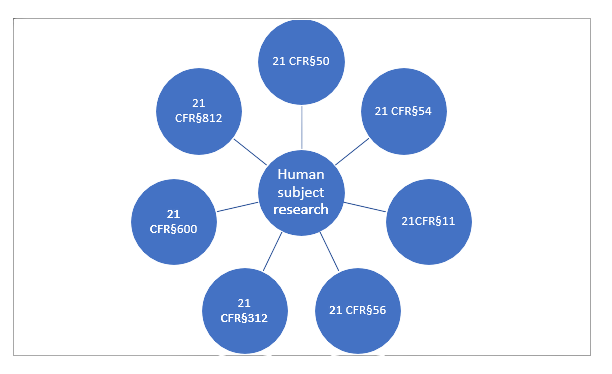
Figure 1 shows the various regulations pertaining the human subjects or clinical research in the CFR which are discussed in detail further.
21 CFR § 50: Protection of Human Subjects
This part relates to all clinical investigations regulated by the FDA and those that support research and marketing permits for products regulated by the FDA. In order to protect the rights and well-being of human subjects in research it is imperative for the investigator to obtain consent from the subject or their legally authorized representative (LAR). Obtaining informed consent is important as it prevents unnecessary coercion and allows subjects to exercise their rights. Listed are exceptions where informed consent cannot be obtained such as life-threatening situations, inability to communicate with the subject or LAR, lack of time, or cases when the investigative product is the best therapy that is available. The various details that are required to obtain informed consent that explains research details,
risk-benefit profile, a list of any untoward reactions or discomfort that is expected and contact information for subjects to contact a representative in case of problems, and a statement of voluntary participation. Also included is information relating to costs to patients, termination, and consequences regarding withdrawal from the study. Documentation requirements, either written or oral consent by the subject or LAR, and requirements of informed consent in case of children by parents or guardians under various circumstances are also outlined in this part.
21 CFR § 54: Financial Disclosure by Clinical Investigators
This section relates to the minimization of bias based on the outcomes of clinical studies in favor of investigators who may have financial interests such as royalty arrangements or patents resulting from the conduct of studies. The FDA is responsible for reviewing disclosure statements, and study designs, and conducting audits and further questioning to assure that data integrity is not affected in any way. Record keeping and maintenance of financial disclosure statements by the applicant’s contracted clinical investigators is of utmost importance and should be accessible to the FDA for verification.
21 CFR § 11: Electronic Records; Electronic Signatures
This part relates to the FDA’s view on the reliability and trustworthiness of electronic records, electronic signatures, and handwritten signatures executed to electronic records to be equivalent to paper records to adopt the widespread use of electronic technology in clinical research. Various recommendations for requirements by the FDA such as validation of computerized systems (accuracy, reliability, integrity, availability, authenticity) and risk assessment in proportion to the safety and integrity of the records, audit trails with date, time, or sequence of events, provision of record copies and access to records to the FDA for inspection, and retention and archival of records are outlined in this part. All steps applicable to the creation and maintenance of electronic records and signatures must be in accordance with predicate rules to ensure compliance with the FDA.
21 CFR § 56: Institutional Review Boards
All clinical investigations for marketing applications for products regulated by the FDA must be reviewed and approved by Institutional Review Boards (IRB). This part contains standards for the composition, operation, and responsibility of IRBs. Instances in which IRB review is required and cases in which it is exempt are clearly stated in these rules. Requirements for IRB registration with the Department of Health and Human Services (DHHS), requirements for registration (name, mailing address, and street address of the institution operating the IRB and each member details, number of protocols, and description of products), details regarding place and time of registration, as well as composition and membership requirements of the IRB are explained. Functions of IRB according to written procedures regarding review of research and approval to ensure human subject safety, and prompt reporting in cases of safety risks or nonadherence to protocols are also outlined. IRBs’ responsibilities and authority to approve or disapprove research as well as require modifications to it, require documentation of informed consent, conduct the continuous review of research, and provide an expedited review in certain instances are stated. Good documentation practices for the maintenance of records and reports by the IRB of research proposals, meetings, correspondences, lists of IRB members, and minutes of meetings should be retained by the IRB and available for inspection by the FDA. Administrative actions by the FDA for noncompliance with regulations by the IRB and the necessity for corrective actions as well as instances of disqualification of an IRB and the institution by the FDA are also a part of this chapter to protect the rights and welfare of human subjects that are part of clinical studies. This regulation ensures that clinical research courses conducted in the United States are conducted ethically and in accordance with the highest standards of safety. The regulation also defines the roles and responsibilities of IRBs, as well as their duties and obligations to protect human subjects involved in clinical research.
21 CFR § 312: Investigational New Drug Application
This part contains the procedures and requirements for submission and approval of Investigational New Drug (IND) applications for initiation of clinical trials in human subjects. Information related to the labeling, promotion, and charging of investigational drugs. The requirements of an IND, the various phases of investigation under which an IND is to be submitted and the information that is reviewed by the FDA in each part is also included. The content and format of an IND application are detailed and should include the following: cover sheet (Form 1571), table of contents, introductory statement and general investigational plan, investigator’s brochure, protocol, chemistry, manufacturing, and control information, pharmacology and toxicology information, previous human experience with an investigational drug, and any additional information. Conditions for and requirements of amendments to protocols and information are stated in this part. Safety reporting including IND safety reports that are submitted periodically, findings from other studies, and animal/in vitro testing should also be provided by the sponsor and any follow-up reports should be submitted to the FDA. Brief reports that include a summary and the status of each study should also be given. Conditions for requests for modifications, clinical holds, termination of IND, and inactive status are specified. Meeting schedules between the FDA and sponsor for discussion and dispute resolution should be held in a timely manner to allow for immediate action to be taken. Responsibilities of sponsors regarding the selection of suitable investigators and monitors, review of investigations, adequate recordkeeping and retention, and investigator roles are described.
21 CFR § 600: Biological Products: General
21 CFR § 600 is a regulation issued by the US Food and Drug Administration (FDA) that establishes standards for biological clinical trials. This part is related to the standards required for the handling, testing, and manufacture of biological products which include virus, therapeutic serum, toxin, antitoxin, vaccine, blood, blood component or derivative, allergenic product, protein, or analogous products, and arsphenamine or its derivatives. Requirements for personnel such as training and qualifications, physical establishment, equipment, animals, and care, record maintenance and retention, reporting of deviations by manufacturers, establishment inspections, adverse events and post-marketing reporting of adverse experiences, and disruption of manufacturing are described in detail.
21 CFR § 812: Investigational Device Exemptions (IDE)
This part is related to the requirements for clinical investigations on devices intended for human use. Labeling requirements, prohibition of promotion of the device by sponsors, requests for waivers, and import and export requirements are stated. The procedure for IDE application and administrative actions including submission of investigational plans, report of prior investigations, and data from clinical studies outside the United States are required. FDA actions such as approval, disapproval, or modifications are included with submission requirements for each. Circumstances for the treatment use of investigational devices and the requirements for the same are enlisted. Selection and roles of investigators and monitors by sponsors are described and IRB compositions, functions, and duties are required prior to IDE. Record and report maintenance and archival and inspections by the FDA are authorized.
Thus, any clinical study carried out in the United States is subject to the above regulations and should be performed in accordance with them to ensure that subject’s safety and well-being is always of prime importance. It is the sponsor’s responsibility to be well-versed with and comply with the various chapters in the Code of Federal Regulations to allow for the smooth conduct of clinical trials for drugs, biologicals, and medical devices that lead to their approval and marketing authorization.
References
1) eCFR :: 21 CFR Part 50 — Protection of Human Subjects
2) eCFR :: 21 CFR Part 54 — Financial Disclosure by Clinical Investigators
3) Part 11, Electronic Records; Electronic Signatures – Scope and Application | FDA
4) eCFR :: 21 CFR Part 56 — Institutional Review Boards
5) eCFR :: 21 CFR Part 312 — Investigational New Drug Application
6) eCFR :: 21 CFR Part 600 — Biological Products: General
7) eCFR :: 21 CFR Part 812 — Investigational Device Exemptions






