This article has been reviewed according to Science X's editorial process and policies. Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Chronic fatigue syndrome is associated with distinct changes in the microbiome
Over the past three years, the emergence of long-term effects associated with COVID-19 has led to increased focus on a disease with similar hallmarks and symptoms—myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). Two studies publishing February 8 in the journal Cell Host & Microbe are taking a closer look at ME/CFS as it relates to the microbiome and the metabolites that microbial species produce.
Both studies found that ME/CFS is associated with reduced levels in the gastrointestinal microbiome of microbes known to produce the fatty acid butyrate. These microbiome disruptions could explain in part how the immune system becomes disrupted in people with ME/CFS.
"It's important to note that this research shows correlation, not causation, between these microbiome changes and ME/CFS," says Julia Oh, an associate professor at the Jackson Laboratory and senior author of one of the two papers. "But these findings are the prelude to many other mechanistic experiments that we hope to do to understand more about ME/CFS and its underlying causes."
"This research demonstrates that there are robust bacterial signatures of gut dysbiosis in individuals with ME/CFS," says Brent L. Williams, an assistant professor at Columbia University and senior author of the other paper. "It helps to expand on this growing field of research by pinpointing the structural and functional disturbances in the microbiome in a chronic disease that affects the quality of life of millions of people."
ME/CFS is a chronic, complex, and systemic disease associated with neurological, immunological, autonomic, and energy metabolism dysfunctions. It has been recognized for decades, but its causes remain poorly understood. Like long COVID, it is believed in most cases to be triggered by exposure to viruses or other infectious agents.
One thing that's made ME/CFS difficult to study is that it tends to be heterogenous—not all people with the disease have the same medical history or symptoms. Both research teams say that's why it's important to do studies like these that analyze data from a large number of patients. The microbiome has recently emerged as a potential contributor to and biomarker for ME/CFS, making it important to study.
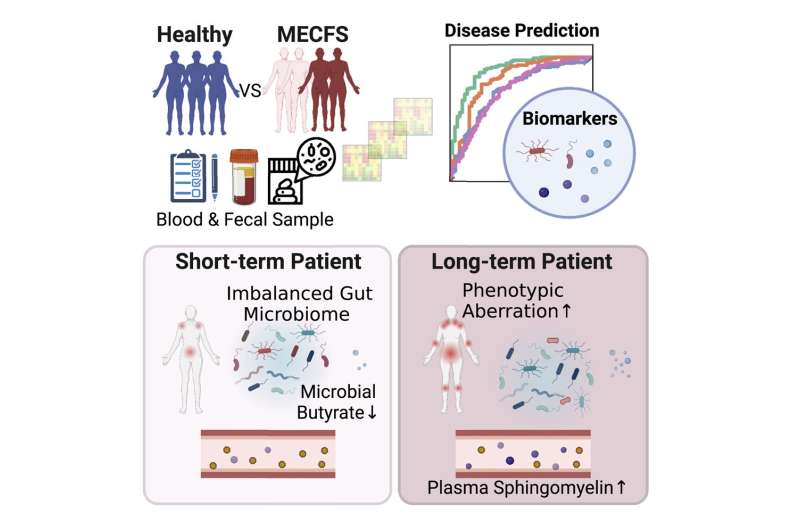
Oh's study used shotgun metagenomics to compare microbiome samples from people with both short-term ME/CFS (defined as those diagnosed in the previous four years; 74 patients) and long-term ME/CFS (defined as those who have had symptoms for more than 10 years; 75 patients) as well as 79 age- and sex-matched healthy controls. The investigators also looked at plasma samples from the participants. The patients were being treated at the Bateman Horne Center in Salt Lake City, Utah, which has a longstanding collaboration with members of the Jackson Laboratory.
The analysis showed that patients with short-term disease had a number of changes to their microbiomes with regard to diversity. Most notably, they had a depletion of microbes known to be butyrate producers. Butyrate is important for protecting the integrity of the gut barrier and is also known to play an important role in modulating the immune system.
In contrast, those with long-term disease had gut microbiomes that had reestablished and were more similar to the healthy controls. However, those participants had accumulated a number of changes in the metabolites in their blood plasma, including many of those related to the immune system. They also had differences in levels of certain types of immune cells compared with the healthy controls.
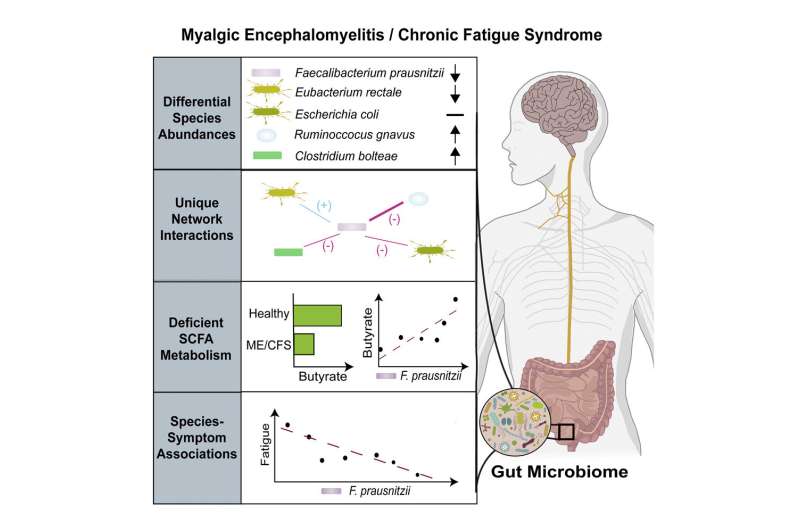
Williams's study used shotgun metagenomic sequencing to look at the microbiomes of 106 people with ME/CFS and 91 healthy controls that were matched for age, sex, geography, and socioeconomic status. This study was undertaken by an interdisciplinary, multi-institutional research group, the Center for Solutions for ME/CFS, and recruited patients from five different sites across the United States, which helped to control for microbiome differences that may be present in different geographic regions.
This study also looked at levels of microbial species in the stool. It didn't include analysis of plasma, though this group has already published plasma metabolomics analyses from their cohort elsewhere. It did look at metabolites in the stool, which demonstrated reduced levels of butyrate metabolites in ME/CFS.
The study from the Columbia team found significant relationships between the severity of fatigue symptoms and levels of specific species of gut bacteria—in particular the butyrate-producing bacterium Faecalibacterium prausnitzii. It also revealed a higher overall load of bacteria in the stool and disturbances in the interactions among bacterial species in patients with ME/CFS.
More research is needed before these findings can be applied directly to new treatments, but the researchers say these findings will aid in the development of new diagnostic tools and could help with the development of better animal models.
"While these findings don't unequivocally demonstrate causative relationships between disturbances in the microbiome and symptoms, these microbiome-symptom relationships present potentially actionable, manipulatable targets for future therapeutic trials," Williams says. "These trials could perhaps focus on dietary, probiotic, prebiotic, or synbiotic interventions and could provide direct evidence that gut bacteria influence chronic symptom presentation."
Oh notes that her future studies will help to further subdivide patients by the features of their disease, including those with conditions frequently associated with ME/CFS—like irritable bowel syndrome and neuroinflammatory disorders. "This will help us pinpoint specific microbial and metabolomic factors that are associated with this disease," she says.
Williams plans to further investigate his findings in animal models. "A tractable mouse model to study the gut microbiome disturbances found in ME/CFS would provide an important tool to evaluate causal hypotheses, mechanisms, and treatments," he says.
More information: Julia Oh, Multi-'omics of gut microbiome-host interactions in short- and long-term Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) patients, Cell Host & Microbe (2023). DOI: 10.1016/j.chom.2023.01.001
Brent L. Williams, Deficient butyrate-producing capacity in the gut microbiome is associated with bacterial network disturbances and fatigue symptoms in ME/CFS, Cell Host & Microbe (2023). DOI: 10.1016/j.chom.2023.01.004




















