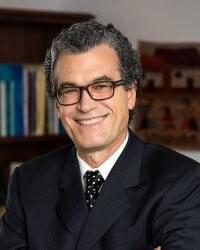
This year’s annual Steering Committee meeting for the NIH Pragmatic Trials Collaboratory featured health equity as a central topic of discussion. In an interview after his keynote presentation, Eliseo J. Pérez-Stable, MD, Director of the National Institute on Minority Health and Health Disparities (NIMHD), shared his thoughts on national priorities for reducing health disparities and opportunities for clinical researchers to help promote health equity.
Pérez-Stable outlined 5 key ways science can help reduce inequities:
- Standardized measurement of social and demographic factors that affect health
- Facilitate discovery science with big data
- Be an engine for promoting diversity of the scientific and clinical workforce
- Cultivate community engagement and build trust for sustainable relationships
- Implement what we know can work to promote health equity
A major theme of his presentation was that a community-engaged approach has to be leveraged in order to get a representative research study. “People just don’t show up because you have a good study. You have to have some kind of community connection,” he said. He recommended sitting down with people as equals to co-develop research. “Don’t come to them with ‘here’s what I’ve got to offer you’—there has to be some evolution of goals during that process.”
Pérez-Stable described the extra effort needed for researchers to build sustainable bonds in communities. “You have to go to the community, go to the stores, be there, and participate, even if unrelated to your research or your studies,” he said. “The saying ‘move at the speed of trust’ is so essential.”
Furthermore, diverse clinical investigators at the principal investigator and co-investigator level really matter in terms of achieving inclusive participation in clinical studies. While there have been some improvements in diversifying the clinical workforce, there has not been enough progress, according to Pérez-Stable.
Similarly, although the research community has made strides in capturing reliable data on participant race and ethnicity, there is still much room for improvement, especially when it comes to electronic health record data in the clinical setting, which is particularly relevant for pragmatic trials. Systematic measurement of race and ethnicity are essential to understanding disparities and providing equitable care. Going forward, there is also tremendous value in capturing more granular data on individuals’ heritage and background.
Finally, Pérez-Stable cautioned that researchers must keep an eye on factors such as the digital divide so health disparities do not get exacerbated. Digital methods are easy for researchers to rely on, but we must remember there is less technology uptake in populations such as older adults, minorities, and the working class. “We can’t just jump to digital methods and expect everyone to join us,” he warned. For example, a significant number of households do not have a computer, and data usage for mobile devices costs money.
Pérez-Stable stated that he is impressed with the work the NIH Collaboratory is doing to bring health equity to the forefront in clinical research, including through the new Health Equity Core, and he hopes the research community will continue to think in terms of what we should be doing to reduce health disparities.
Stay tuned for more interviews with program leaders from the 2023 Steering Committee meeting.


