NS Pharma takes on Sarepta as FDA approves DMD drug
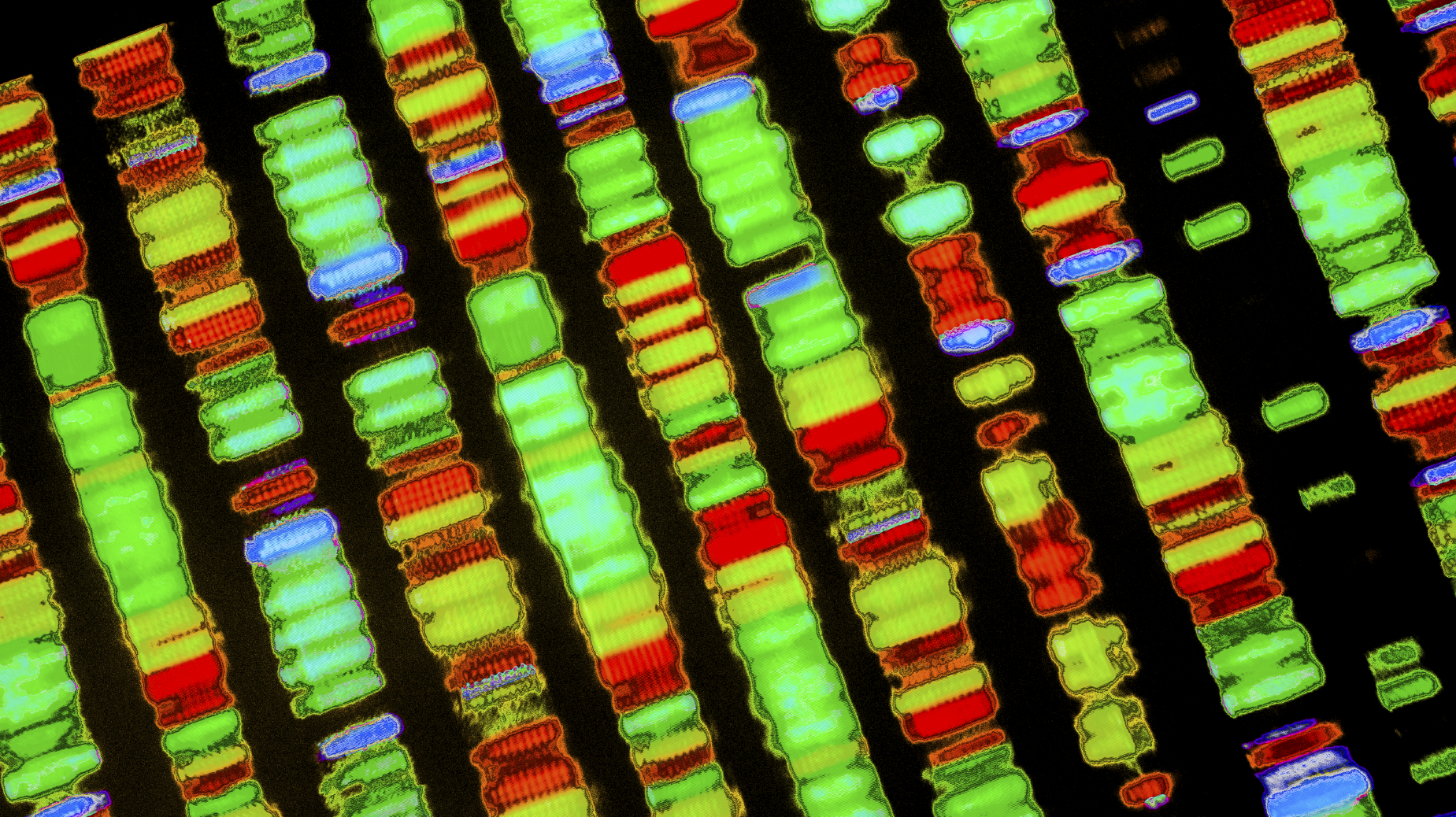
The FDA has approved a new therapy for the rare muscle wasting disease Duchenne muscular dystrophy (DMD) as Japan’s NS Pharma takes on Sarepta and its controversially approved rival. NS Pharma’s Viltepso (viltolarsen) has been approved in patients who have confirmed mutation of the DMD gene that is amenable to exon 53 skipping. The DMD gene is made up of 79 exons, and mutations in that code can result in a deficiency in dystrophin which is responsible for the muscle wasting in DMD. Exon-skipping drugs are used to patch the mutations and allow the gene to produce partially functional dystrophin. Viltepso can be used to treat around 8% of DMD patients and previously approved DMD drugs has not been shown to change the course of the disease. However what it does do is help produce the dystrophin that patients with the disease are lacking. It’s bad form to compare performance of drugs in separate clinical trials, but results suggest that Viltepso helps patients produce more dystrophin than Sarepta’s rival Vyondys 53 (golodirsen). The FDA controversially approved Vyondys 52 late last year after a previous rejection and an appeal from Sarepta. Viltepso was evaluated in two clinical studies with a total of 32 patients, all of whom were male and had genetically confirmed DMD. The increase in dystrophin production was established in one of those two studies, a study that included 16 DMD patients, with 8 patients receiving Viltepso at the recommended dose. In the study, dystrophin levels increased, on average, from 0.6% of normal at baseline to 5.9% of normal at week 25. The FDA deemed that this increase in dystrophin production is “reasonable likely” to predict a clinical benefit –something that is difficult to measure in such a small study. As part of the accelerated approval process, the FDA requires NS Pharma to conduct a trial to confirm clinical benefit. This ongoing study will assess whether Viltepso improves the time to stand for DMD patients with the confirmed mutation. If the trial fails to verify clinical benefit, the FDA may begin proceedings to withdraw approval. The most common side-effects in the two trials were upper respiratory tract infection, injection site reaction, cough and fever. There have been no signs of liver toxicity in the 80 patients treated so far, but the FDA is warning doctors to monitor renal function as this issue has been observed in patients taking antisense oligonucleotides.












